“In this study, inulin supplementation was found to improve bowel symptoms and quality of life but had no superior effect on symptoms of depression and stool type compared to the placebo group,” wrote researchers at Mardin Artuklu University and other institutions in Turkey.
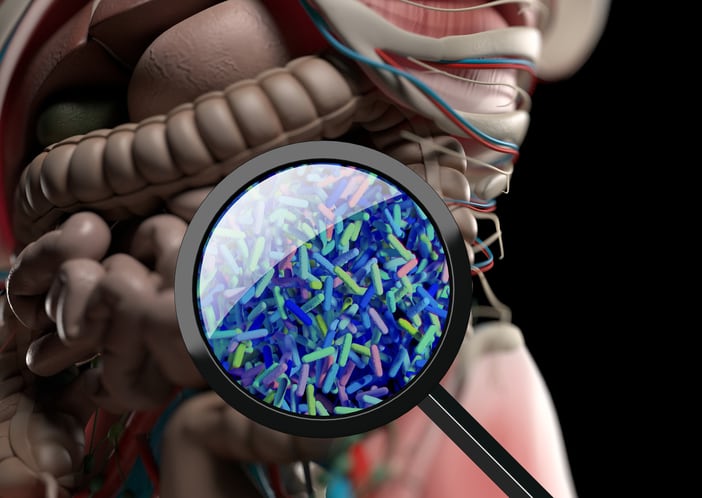
Inulin is a soluble dietary fiber that acts as a prebiotic. In the colon, gut microbiota ferment inulin to produce beneficial metabolites, such as short-chain fatty acids, that support gut health and immunity.
By supporting the microbiota, inulin can regulate colon transit time, stool consistency and the frequency of defecation. In addition, previous studies have suggested that inulin may have beneficial effects on psychological symptoms by modulating the gut microbiota through the brain–gut axis.
Because stress is implicated in the pathophysiology of IBS, the researchers hypothesized that inulin may positively affect both physical and psychological symptoms in people with IBS-C.
“It may be appropriate for individuals with IBS to be aware of their disease, to apply lifestyle changes, to determine the topics to be regulated in their diet, to encourage physical activity and to provide psychological support to reduce their stress in order to manage the disease, reduce symptoms and improve quality of life after diagnosis,” the researchers wrote.
Additionally, they noted that a dietitian should supervise dietary restrictions to avoid nutrient deficiencies.
Study details
Researchers randomly assigned 34 adult IBS-C patients from the Gastroenterology Department Clinic of Mardin Education and Research Hospital to receive either a prebiotic containing a total of 9.2 g of equal measures of inulin and oligofructose or a placebo, administered in two daily doses for eight weeks.
The researchers employed questionnaires, appropriate scales and face-to-face interviews to evaluate the primary outcomes of changes in IBS symptoms, depression and quality of life. They also used the Bristol stool scale and the IBS-Visual Analogue Scale (IBS-VAS) to assess symptoms. Evaluation was conducted at the start of the study, in the second month and at the end of the study.
The findings revealed that in the prebiotic group, the IBS-Quality of Life Scale (IBS-QoL) scores increased, and the IBS-Symptom Severity Score Scale (IBS-SSS) score decreased. The prebiotic group had improvements in abdominal pain, bloating and dissatisfaction with defecation habits.
The prebiotic group also showed significant improvements in IBS-VAS parameters of constipation status and psychological state, although there was no superior effect of supplementation on depression symptoms.
The study noted that “stress was found to be the most common factor affecting the progression of IBS,” affecting 58.8% of the prebiotic group and 70.5% of the placebo group.
In conclusion, the researchers recommended a multi-model approach to IBS-C that includes psychological therapies, dietary strategies and lifestyle changes.
They also acknowledged the limitations of the study, which included the inability to evaluate the effects of varying amounts of inulin and oligofructose, as well as a lack of stool samples to assess the microbiota.
Source: Sci Rep 15, 34252 (2025). https://doi.org/10.1038/s41598-025-16321-w, “A randomized trial of inulin for bowel symptoms, depression and quality of life in constipation predominant IBS.”, Authors: C. Akcali et al.