Writing in Nature Biomedical Engineering, the team outline a synthetic biology approach in which the resulting eLBP could offer protection against the effect of β-lactam antibiotics on the gut.
“In designing the eLBP, we tapped into the synthetic biology took kit that we have advanced over the past two decades and enabled Lactococcus lactis, a safe-to-use microbe, to secrete a β-lactamase enzyme that altruistically degrades β-lactams in the bacteria’s environment,” explains lead author James Collins, Termeer Professor of Medical Engineering & Science at MIT.
“The enzyme essentially becomes a ‘common good’ that cannot confer a selective advantage to the producing bacteria or be easily transferred to other bacteria, minimising the risk and maximising the clinical benefits of our approach.”
Splitting genes
In order to prevent antibiotic resistance, the team began engineering control units into the β-lactamase expression system splitting a specific β-lactamase-encoding gene.
These two genetically unlinked halves were then sent to different parts of the bacterium’s DNA.
The halves were then further modified so they would be secreted away from the producer cell later to join together as a functional enzyme.
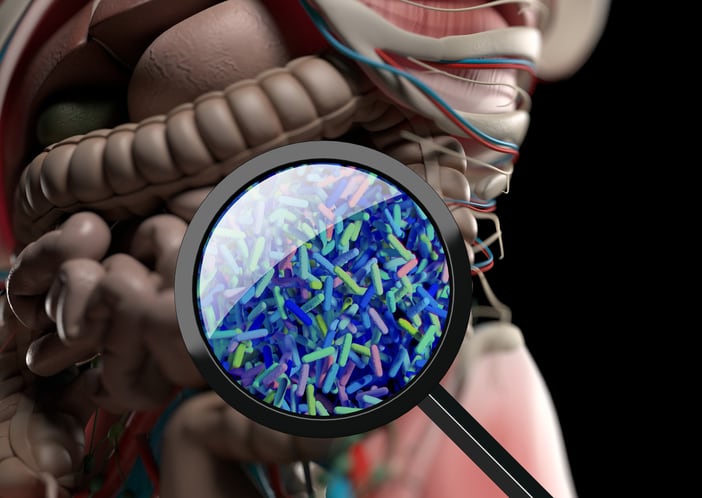
Along with first-author Andrés Cubillos-Ruiz, the team then gave the eLBP to mice along with the antibiotic ampicillin where minimal dysbiosis was observed in the animal’s gut.
By sequencing part of the bacterial genome, they found the eLBP reduced the reduction of microbial populations letting them build up to their original numbers and diversity following antibiotic treatment.
Mice treated with the antibiotic and not given the eLPB, suffered larger microbial diversity losses which could not be recovered during the duration of the experiment.
Hostile takeover
“Importantly, during its transient stay in the digestive tract, the eLBP protected the microbiome without changing the concentration of ampicillin circulating in the blood, which is important because the antibiotic still needs to reach infections everywhere else in the body to do its job,” says Cubillos-Ruiz.
“The eLBP also reduced the enrichment of various antibiotic resistance genes within the microbial community, which commonly happens under the selective pressure of antibiotics.”
Further experiments saw the team address a common occurrence of dysbiosis, namely the hostile takeover of the vacated intestinal territory by harmful bacteria like Clostridioides difficile.
These bacteria, given the opportunity and conditions, can multiply uncontrollably and play a significant role in inflammation, diarrhoea, and even inflammatory bowel disease.
Here, ampicillin-treated mice were infected with C. difficile spores, with the eLBP successfully preventing the C. difficile’s intestinal colonisation.
This observation contrasted with the unmodified L. lactis strain, which did not produce the split β-lactamase enzyme.
‘Living cellular therapeutic device’
“We are now focusing on getting these living therapies to patients and are finalising the design of an effective, short, and inexpensive clinical trial,” says Cubillos-Ruiz.
“We also believe that our general eLBP approach can be extended into a therapeutic platform that could be applied not only to other antibiotics, but also to address diseases where gut dysbiosis is at the centre.”
Wyss Founding Director Donald Ingber adds that the living cellular therapeutic device could become a “true game changer in the treatment of infectious diseases both by helping to maintain a healthy microbiome in patients treated with antibiotics and, perhaps equally important in the longer run, by preventing the growing problem of antibiotic resistance which is a growing problem worldwide.”
Source: Nat. Biomed. Eng
Published online: doi.org/10.1038/s41551-022-00871-9
“An engineered live biotherapeutic for the prevention of antibiotic-induced dysbiosis.”
Authors: Cubillos-Ruiz, A et al.