In addition, patients had increased faecal levels of the short chain fatty acid (SCFA) isobutyric acid, suggesting increased proteolytic fermentation causing intestinal inflammation.
“To the best of our knowledge, this is the first study dedicated to investigating the relationship between the gut microbiota, the intestinal barrier markers, diet, and the occurrence of depressive symptoms among patients after surgical treatment of morbid obesity,” wrote the authors, led by scientists from Pomeranian Medical University in Szczecin, Poland.
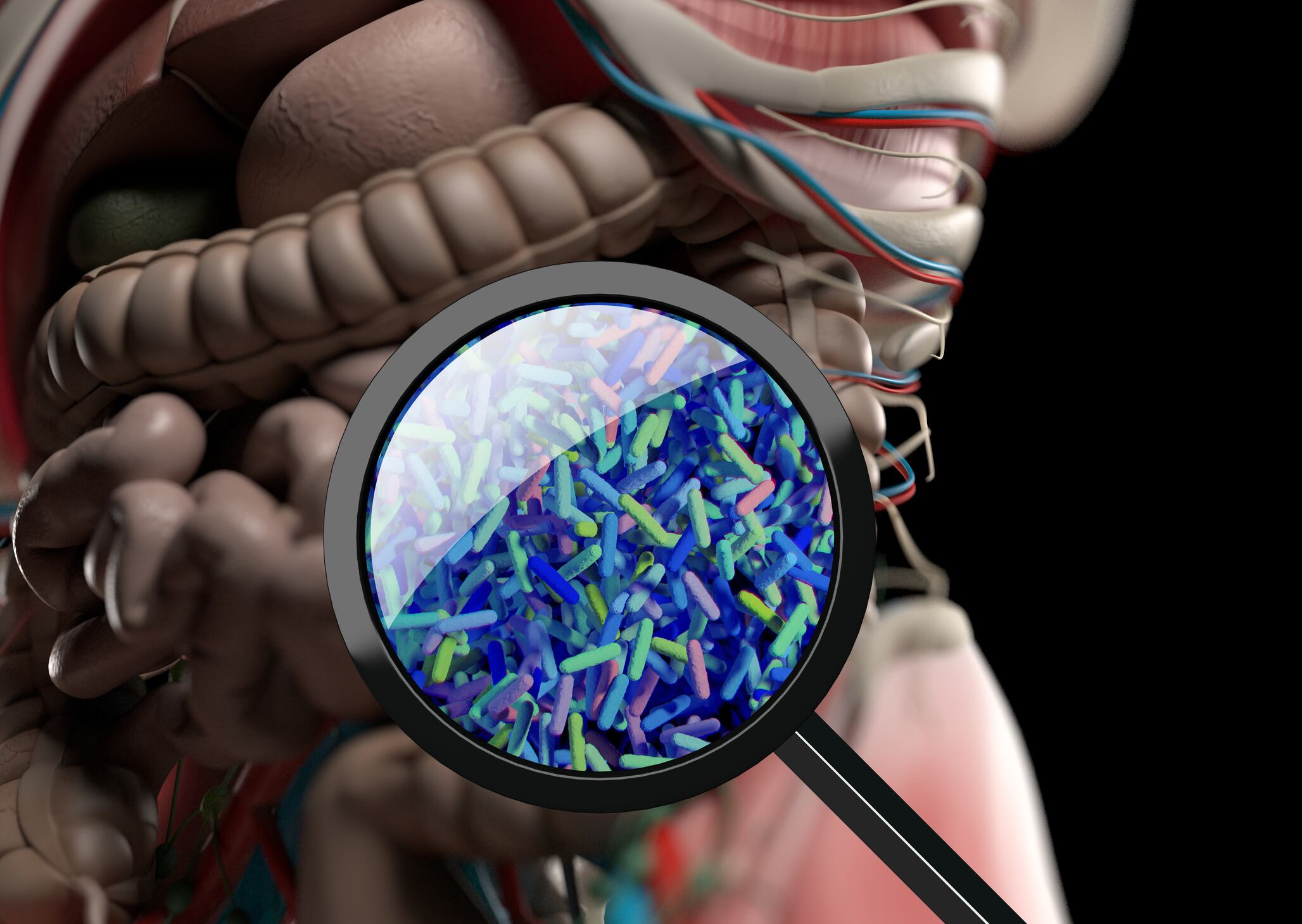
Dysbiosis and depression
Bariatric surgery is an important treatment for those with morbid obesity, often resulting in successful weight loss and significant improvements to quality of life and longevity. Whilst it has been reported that associated depressive symptoms can be alleviated following surgery, some studies have suggested a deterioration in patients’ mental health in the longer term.
Depression and other mental disorders have been associated with gut dysbiosis, with observations noting sufferers had increases in populations of Bacteroidetes and reductions in Firmicutes. Reduced SCFA production and pronounced deterioration in intestinal barrier function has also been noted. In addition, it has been established patients with obesity and subsequent chronic inflammation are more likely to develop depression.
Researchers sought to assess this apparent association of the gut-brain axis and its effects on mood, and the possible associations with mood disorders reported following surgery.
Study details
The study, which is published in Nutrients, included 41 patients, selected on the basis that they had undergone bariatric surgery at least six months prior whilst scoring ≥12 on the Beck scale; a self-assessed questionnaire used to assess depressive symptoms. Following this, biological material, anthropometric measurements, questionnaires, and a food diary for the past 72 hours was collected. A final questionnaire utilising the Hamilton Scale, conducted by an experience psychiatrist, enabled the assessment of the severity of the established depressive symptoms.
The researchers analysed patients’ mental state and microbiota, as well as faecal SCFAs and gut barrier markers.
Overall, it was reported that 67.5% of patients suffered from issues with defecation, as well as a further 40% suffering chronic constipation and 30% with diarrhoea. Of these individuals, species of Enterobacteriaceae, Parasutterella, or Enterococcus were found in significantly higher numbers; those in which have been associated with a range of inflammatory conditions when found in abundance.
Paired with these reported complaints, an association was established between the Beck scale and the SCFAs, with the faecal concentrations of isobutyric acid found to be higher in these patients. Researcher’s highlighted that this finding, paired with a reported low fibre intake, may indicate proteolytic fermentation and its resultant colonic inflammation.
Mood mechanisms
The researchers hypothesised that the greater presence of BCFA could be a contributing factor to developing a depressive disorder, stating “an increase in the amount of BCFA in the stool may indicate an increased proteolytic fermentation (a high amount of protein in the large intestine may result from its high intake in the diet and/or malabsorption disorders) leading to the formation of harmful metabolites, i.e., ammonia, p-cresol, phenols, or hydrogen sulfide.
“Therefore, in order to limit proteolytic fermentation, it seems justified to pay special attention to the appropriate dietary fibre intake in the diet of patients after bariatric surgery”, they stressed.
The findings established pronounced differences in the microbiotas following differing bariatric treatments in those suffering with depressive symptoms. Whilst the treatments were found to differ substantially, introducing heterogeneity and reduced validity to the results, the extent of dysbiosis taking place following surgery was highlighted.
The study draws potential parallels between the established dysbiosis, and mood disorders suffered post-surgery. Yet, the small sample size paired with established confounders emphasises the need for study replication utilising RCTs to investigate this possible relationship further.
Source: Nutrients
2022, 14(24), 5372 https://doi.org/10.3390/nu14245372
“Association between Fecal Microbiota, SCFA, Gut Integrity Markers and Depressive Symptoms in Patients Treated in the Past with Bariatric Surgery—The Cross-Sectional Study”
Authors: N. Komorniak ety