‘Natural prebiotic’ in breastmilk may shape iron supplement effects on gut microbiome

Writing in the journal Nutrients, the research team concludes that infants of non-secretor mothers (unable to produce certain HMOs) may be more vulnerable to the adverse effect of fortificant iron on the gut microbiota.
This could result in decreased numbers of Bifidobacterium and increased numbers of harmful enteropathogens, say the Swiss scientists, who also worked alongside NIZO Food Research in The Netherlands.
The team suggests these children could benefit more from the Galacto-Oligosaccharide (GOS) sugars in terms of beneficial effects on the gut microbiota and improving iron status.
“The differing breast milk Human Milk Oligosaccharide (HMO) profile of secretor and non-secretor mothers appeared to modulate the impact of the iron and GOS intervention,” the study says.
“Infants in the Iron (Fe) group and of non-secretor mothers were particularly vulnerable to the decrease in abundance of Bifidobacterium and to the increase in the sum of all pathogens.
“However, infants of non-secretor mothers (NS) benefited the most from the co-provision of GOS (FeGOS-NS group) in maintaining high abundances of Bifidobacterium and reducing enteropathogens.”
HMO prebiotic
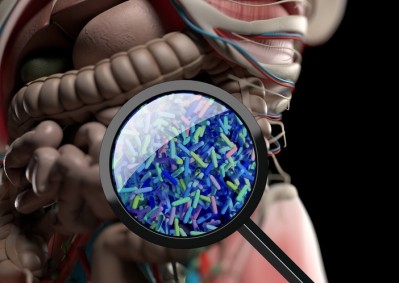
Human milk oligosaccharides (HMOs) represent the third most abundant solid milk component after lipids and lactose in human breast milk, with a concentration of 5–10 grams per litre (g/L) and more than 200 different structures.
The HMO composition of breast milk varies between mothers, differs across geographic regions, and changes over the course of lactation.
Most HMOs are not absorbed in the gastrointestinal tract of the breastfed infant and reach the colon intact, where they can act as prebiotics.
Studies show that Bifidobacterium spp., with strain specific ability, and Bacteroides spp., both express enzymes for efficient use of HMOs as a carbon source.
To treat or prevent iron deficiency anaemia (IDA) many infants in low-income countries receive iron fortificants between 6–24 months of age.
However, iron is an essential micronutrient for most gut bacteria and is important for virulence and colonisation of potential enteropathogens.
As ‘natural prebiotics’, HMOs could provide similar protection from the adverse effects of iron fortificants on the infant gut microbiota, and these protective effects could depend on specific HMO composition of breast milk and maternal secretor status.
Study methods
Along with Nizo Research, investigators from the ETH Zurich, Jomo Kenyatta University in Kenya and the University of Zurich, began looking at data from 75 mother–infant pairs enrolled on a four month intervention trial.
The infants, aged 6.5–9.5 months, were spread over three intervention groups that received no iron or GOS, iron only, or iron and GOS.
The supplements were supplied to the mothers in the form of a daily sachet containing a micronutrient powder, which could be added to the infants’ food.
HMO composition analysis in maternal breast milk to determine secretor status found 28% of mothers were non-secretors indicating regional secretor prevalence (72%) may be higher than average.
HMO profiles of maternal breast milk samples showed differences between the secretor and non-secretor mothers.
When the infants’ stool samples were analysed for selected pathogenic bacteria, maternal secretor status was found to have no impact on the composition of the infant gut microbiome.
Researchers then looked at the three intervention groups and found in the ‘no iron or GOS’ control group, the infants of non-secretor mothers were more likely to get diarrhoea.
In the ‘iron only’ group, the infants of non-secretor mothers had a greater decrease over the four-month period in the relative abundance of protective bacteria.
Finally, in the ‘iron and GOS’ group, infants of non-secretor mothers benefited the most from the co-provision of GOS.
These infants maintained protective bacteria, and had a significant increase in body iron stores over the four-month period, while no such increase was seen in the infants of secretor mothers.
Higher viral infection risk
“Our findings show that maternal secretor status does not have a major impact on the gut microbiota of the mothers,” says the team, led by Dr. Daniela Paganini and Professor Michael Zimmermann at ETH Zurich, Switzerland.
“Previous studies have linked maternal secretor status to a higher risk for viral infections, including norovirus, rotavirus and respiratory viruses in women.
“In contrast, maternal non-secretor status has been linked with symptomatic enterotoxigenic Escherichia coli (ETEC) infection in women.
“In our study, there were no differences in abundance of enteropathogens comparing secretor to non-secretor mothers, with the exception of higher C. perfringens among non-secretor mothers.”
The team recommends future studies would be valuable to investigate the effect of specific HMOs on iron absorption and their effects on the gut microbiota when given with fortificant iron.
Source: Nutrients
Published online: doi.org/10.3390/nu11112596
“Maternal Human Milk Oligosaccharide Profile Modulates the Impact of an Intervention with Iron and Galacto-Oligosaccharides in Kenyan Infants.”
Authors: Daniela Paganini et al.