Metabolic complications blunt benefits of probiotics on depression, data suggests
The trial missed its primary goal as a probiotic proved no more effective than placebo at relieving depression symptoms over 60 days of treatment.
However, a subgroup of participants that responded very well to the treatment tended to have a lower body mass index (BMI) than others in the same group, with average scores of 23.17 and 25.07, respectively. They also had a lower hepatic steatosis index and a lower quality of life score, the researchers observed.
Commenting independently on the study, Glenn Gibson, a professor of food microbiology at the University of Reading, UK, said that the research was “very well conducted and described” regarding which types of probiotics might help in treating depression. Using another species of bacteria and prebiotics could have provided more enhanced effects, he added.
‘Add-on treatment’ for depression
Depression, which involves lowered mood levels and a loss of energy, affected 280 million people around the world in 2019, including 5% of all adults. This condition alone costs the global economy around $1 trillion in lost productive days and is linked to metabolic syndrome disorders including obesity, hypertension and insulin resistance.
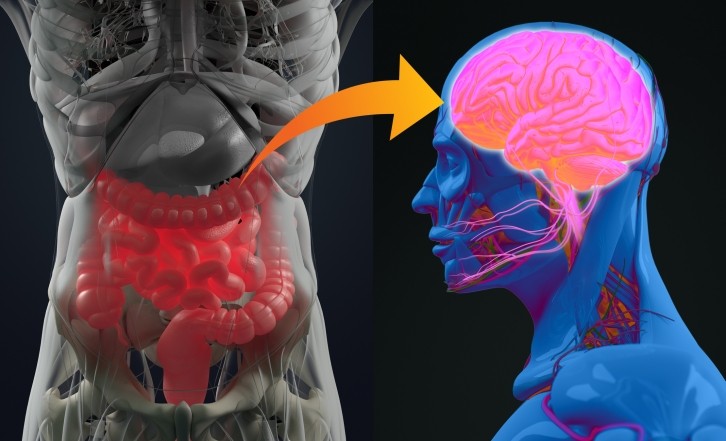
The gut microbiome plays a role in modulating mental health via the microbiota-gut-brain axis, and probiotic treatments have often been studied as potential strategies for tackling depression. In general, however, the treatments have only been effective as an add-on therapy, according to the researchers on the current study.
Their double-blind controlled trial enrolled 95 participants (mean age of 34.4 years, 85.3% women and 95% of Caucasian) in Poland who had been diagnosed with depression based on the 11th International Classification of Diseases (ICD-11) and with a score of 13 or more on the clinician assessed Montgomery–Asberg Depression Rating Scale (MADRS) score, which ranges from 0 to 60 where a higher score indicates more severe symptoms.
The cohort had a mean body mass index (BMI) of 24.88 kg/m², while 56.8% and 24.2% of subjects had abdominal obesity and metabolic syndrome, respectively, according to International Diabetes Federation guidelines.
Participants were assigned to take either a capsule containing Lactobacillus helveticus Rosell-52 and Bifidobacterium longum Rosell-175 (3 × 109 colony forming units plus excipients) or a placebo (excipients only), with group sizes of 51 and 44, respectively. The investigators then tracked psychometric progress over 60 days.
The treatment and placebo groups showed no significant difference in improving depression symptoms with respective mean drops of 4.9 and 3.7 points on MADRS, the trial’s main outcome measure. However, the investigators observed that significantly more participants given the probiotic achieved an improvement of at least two points in the MADRS.
In addition, there were “interesting correlations” between metabolic measures such as BMI and hepatic steatosis index and the improvement in depression symptoms in the treatment group as measured using the self-assessed Depression, Anxiety, Stress Scale (DASS), the researchers noted.
“We hypothesize that more severe or functionally different forms of dysbiosis connected with higher rates of central fat storage require different or more advanced interventions,” the wrote. “These may include multi-strain probiotic formulations, longer durations of supplementation, or different strains of probiotics.”
More advanced probiotics
Amy Reichelt, chief innovation officer at Canadian neuroscience company PurMinds, who was not involved in the study, said that inflammation can be a cause of depression in a subset of individuals but not everyone.
“A more advanced intervention could be the combination of a probiotic, diet plan focused on anti-inflammatory foods, for example the Mediterranean-diet and an exercise regime, coupled with anti-depressant treatment,” she said.
Some of the main challenges in developing probiotic treatments for depression involve getting the right mix, with a wide range of options of species, prebiotics and encapsulation technology available.
''The main challenge is that everyone’s gut microbiome is unique like a fingerprint,” Reichelt said. Microbes in probiotics also need sustenance in the form of prebiotic fiber, so taking probiotics alone has a limited effect, she added.
The future of probiotic research in depression involves establishing solid evidence of efficacy and using a precision medicine approach, experts say. For example, Reichelt suggests conducting “gut microbiome sequencing analysis on individuals prior to undergoing a treatment to identify ‘gaps’ where specific probiotic interventions might have the best effects.''
Source: Nutrients
2024, 16(9), 1389, doi: https://doi.org/10.3390/nu16091389
"Metabolic Status Influences Probiotic Efficacy for Depression—PRO-DEMET Randomized Clinical Trial Results"
Authors: Oliwia Gawlik-Kotelnicka et al.












