Writing in Gut, gastroenterology experts recommend the use of probiotics as a first-line treatment although they stopped short of recommending a specific species or strain.
“It is reasonable to advise patients wishing to try probiotics to take them for up to 12 weeks, and to discontinue them if there is no improvement in symptoms,” the guidelines add.
Along with probiotics, the paper’s authors also point to simple dietary changes as well as adopting healthy eating patterns as beneficial to IBS patients.
The guidelines also extend to the reduction of dietary fibre to improve symptoms, although the team also acknowledge others may find a soluble fibre supplement helps.
What is IBS?
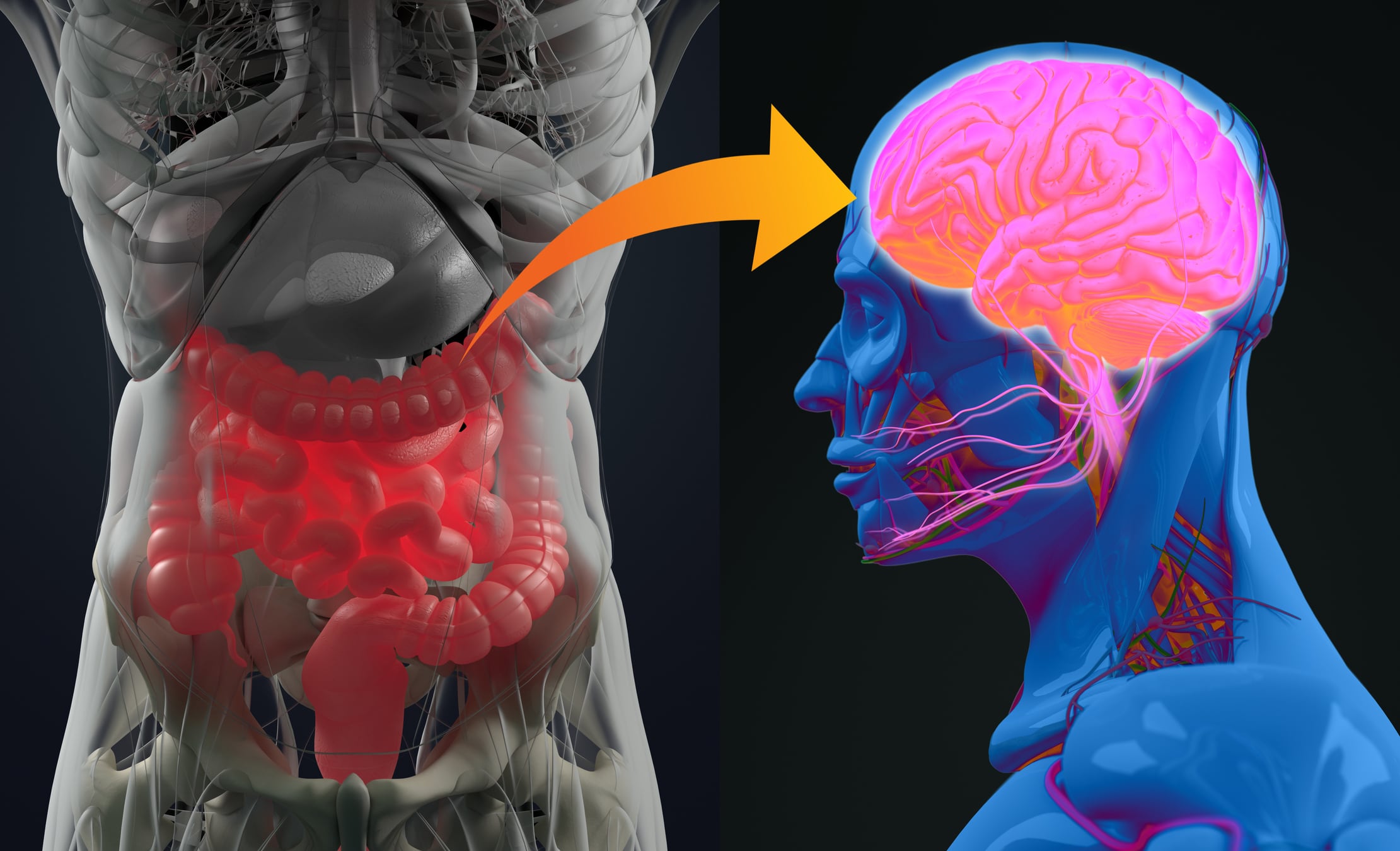
IBS is a condition caused by problems arising between the gut and the brain. It consists of symptoms such as abdominal pain linked to changes in bowel frequency or appearance of stools, and often bloating.
Problems in IBS have been found in the nervous system supplying the gut, often making it more sensitive.
Psychological factors (including stress), certain foods and the micro-organisms living in the gut can all play a role in triggering symptoms.
Occasionally, it can start after a gut infection, or antibiotic use, but more often there is no clear origin.
In summarising research looking into probiotics’ possible usefulness in addressing IBS, the team updated a prior meta-analysis of 37 Randomised Controlled Clinical Trials (RCTs), including data from 8 new trials and randomising 6352 patients.
Analyses of probiotic type demonstrated significant effects on global symptoms or abdominal pain for combinations of probiotics, Lactobacillus, Bifidobacterium and Escherichia.
While the study noted similar adverse event rates in the probiotic and placebo arms, variations in study design, strain and species of probiotic used, and heterogeneity between studies make it difficult to give specific recommendations.
Along with probiotics, the guidelines also identify soluble fibre, such as ispaghula, as an effective treatment for global symptoms and abdominal pain in IBS.
Insoluble fibre such as wheat bran however should be avoided as it may exacerbate symptoms, according to the paper’s authors.
The team also recommends that soluble fibre should be started at a low dose (3–4 grams per day (g/day)) and built up gradually to avoid bloating.
Other potential treatments for IBS includes a diet low in fermentable oligosaccharides, disaccharides and monosaccharides and polyols, as a second-line dietary therapy.
Supervised by a trained dietitian
The team acknowledges this approach as an ‘effective treatment for global symptoms and abdominal pain in IBS, but its implementation should be supervised by a trained dietitian and fermentable oligosaccharides, disaccharides and monosaccharides and polyols should be reintroduced according to tolerance.’
“With regard to fibre, a systematic review and meta-analysis of 15 RCTs, comprising 946 patients, demonstrated its benefit in IBS.
“However, this effect was limited to soluble fibre, such as ispaghula but not insoluble fibre, like wheat bran, which may exacerbate abdominal pain and bloating.
“It is generally advised to start with low doses of soluble fibre (3–4 g daily) and build up gradually, as tolerated, to a total dosage of 20–30 g/day, as it increases colonic water content and volume, which may aggravate abdominal pain and bloating,” the team states.
The guidelines’ fibre recommendations form part of a broader dietary approach in which adopting healthy eating patterns, such as regular meals, maintaining adequate nutrition, limiting alcohol and caffeine intake, adjusting fibre intake, and reducing consumption of fatty and spicy foods was advised.
However, the paper acknowledges that evidence for this is based on a combination of clinical experience and the potential mechanisms by which these foods may induce gastrointestinal symptoms in IBS, rather than evidence from RCTs of this approach versus a control treatment.
Source: Gut
Published online: doi.org/10.1136/gutjnl-2021-324598
“British Society of Gastroenterology guidelines on the management of irritable bowel syndrome.”
Authors: Vasant DH et al.