Whether there should be mandatory fortification of folic acid across the EU has been hotly debated for some time, with regulatory agencies across the bloc pondering the idea of introducing national guidelines for fortification of foods with the pro-vitamin.
NutraIngredients rounds up mandatory and voluntary folic acid fortification efforts in Europe and beyond.
The UK: Fortification on the cards?
The only EU country moving in the direction of mandatory fortification is the UK.
Currently, UK flour is enriched with nutrients such as iron, calcium carbonate and thiamin (vitamin B1) and there is strong support for adding folic acid to this list.
The Scientific Advisory Comittee on Nutrition (SACN) and food standards groups including the Food Standards Agency in Scotland and Northern Ireland have recommended mandatory fortification of flour with folic acid and the decision is now in the hands of UK health ministers.
The Scottish government is strongly committed to mandatory fortification and, in the absence of firm commitment from Westminster, is taking steps towards mandatory fortification on a Scotland-only basis.
Ireland: Voluntary approach failing
Ireland came close to implementing mandatory flour fortification on the back of a recommendation by the Food Safety Authority of Ireland (FSAI) in 2006.
Three years later, the programme was halted when mandatory flour fortification was deemed unnecessary. Instead, voluntary fortification was pursued to bring NTD rates down.
However, according to a study published last year in the Journal of Public Health, the percentage of fortified foods has since decreased, and the incidence of neural tube defects is increasing.
According to Professor Helene McNulty, director of the Northern Ireland Centre for Food and Health (NICHE), this has put the spotlight back onto mandatory fortification.
“Ireland is probably the closest country to the UK (within Europe) in terms of considering mandatory folic acid fortification.
"The decision is now in the hands of the government health minister,” she told NutraIngredients.
Rest of Europe and Asia: Resistant to fortification
In other European countries, mandatory fortification looks unlikely to happen any time soon, with most governments preferring to rely on public health recommendations for folic acid intakes as a means of preventing NTDs.
Advice differs between countries, although the majority follow the World Health Organisation (WHO) guidance of a healthy diet plus a folic acid supplement of 400 micrograms per day from preconception (4-12 weeks) until the end of the first trimester of pregnancy (8-12 weeks).
Three European countries - Finland, France and Sweden - consider supplementation unnecessary if a healthy diet is adhered to.
Singapore and Taiwan have taken a similar stance, and Asian countries in general are unlikely candidates for mandatory folic acid fortification, with fortification efforts focused on other nutrients.
The US: Where it all started
The US became the first country to introduce mandatory folic acid fortification in 1998, a policy which has resulted in a decline in NTDs.
According to data from the US Centers for Disease Control and Prevention, NTD prevalence decreased by 36% after fortification, although prevalence was 21% higher among Hispanics.
This led to an FDA announcement last week that the mandate would be extended to include corn masa flour - a staple in Hispanic diets.
Successful mandatory fortification programmes have also been documented in other countries including Canada, Costa Rica, Chile and South Africa, resulting in significant increases in blood folate concentrations and 25-50% reductions in the prevalence of NTD-affected pregnancies.
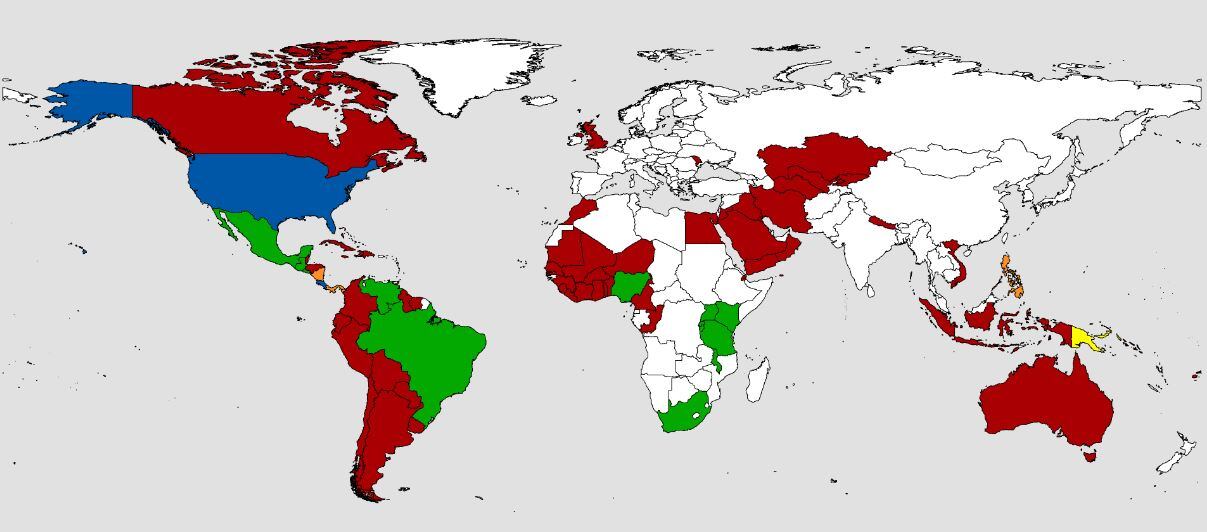
Post-Soviet states embrace fortification
The former Soviet Union countries have also proved willing adopters of mandatory fortification. Turkmenistan was one of the first countries to fortify its flour supplies in 2006, a policy that has resulted in lower NTDs.
Other post-Soviet countries including Kazakstahn, Kyrgyzstan and Uzbekistan have since followed suit, and others, such as Tajikistan and Georgia, are planning to implement mandatory fortification.
Australia and New Zealand: Differences down under
In 2009, Australia and New Zealand jointly agreed on mandatory fortification.
However, whilst Australian millers have been adding folic acid to wheat flour used for breadmaking at a dose of 2–3 mg per kilogram since 2009, just one month before the planned introduction of folic acid fortification the New Zealand government announced it would not be going ahead with the deal signed by the two countries two years earlier.
The government’s minister of health said further research was needed and the decision was deferred. In 2012 the government made a decision to continue with voluntary fortification of bread with folic acid rather than making it mandatory.
