The study, conducted by researchers at Setsunan University, Mizkan Co., Ltd. and Kyoto Prefectural University of Medicine, collected data on 105 adults aged 20 to 50.
They consumed either low-fibre control foods providing about 2.2g of total daily fibre (including 1.2g of fermentable fibre per day) or high-fibre foods delivering about 8.2g of total fibre daily (with 6.4g per day of fermentable fibre) on top of their usual diets.
The intervention ran from August 29 to September 26, 2024.
Outcomes were assessed at baseline, week two, and week four.
The team tracked stool diaries, bowel-related quality of life using the validated Japanese Patient Assessment of Constipation Quality of Life (JPAC-QOL), sleep using the OSA-MA inventory, self-reported skin condition, faecal organic acids, and gut microbiota via 16S rRNA sequencing.
Bowel-related quality of life improved within two weeks
Participants received seven pre-portioned products per week — two cereals, two teas, one cookie, one portion of noodles, and one waffle — mirroring realistic product sizes and taste profiles.
Both groups improved in terms of JPAC-QOL over four weeks but the high-fibre group recorded larger effect sizes, especially on the overall score.
Participants reported less physical discomfort, fewer worries or concerns related to constipation, and greater satisfaction with bowel habits.
Several question-level improvements appeared only in the high-fibre arm at both week two and week four, suggesting a dose-response effect.
Stool diary measures supported these perceptions.
From baseline to weeks two and four, participants reported more bowel movements per week, more days with a bowel movement, and greater stool amount per movement.
These changes appeared earlier and more strongly in the high-fibre group.
Stool form scores did not worsen, indicating that a higher fibre intake improved frequency and volume without pushing consistency in an undesirable direction.
This meant that a realistic food-based fibre load near 8g of additional total fibre daily — roughly 6g per day as fermentable fibre — can improve consumer-relevant outcomes within two weeks, with benefits sustained through a month.
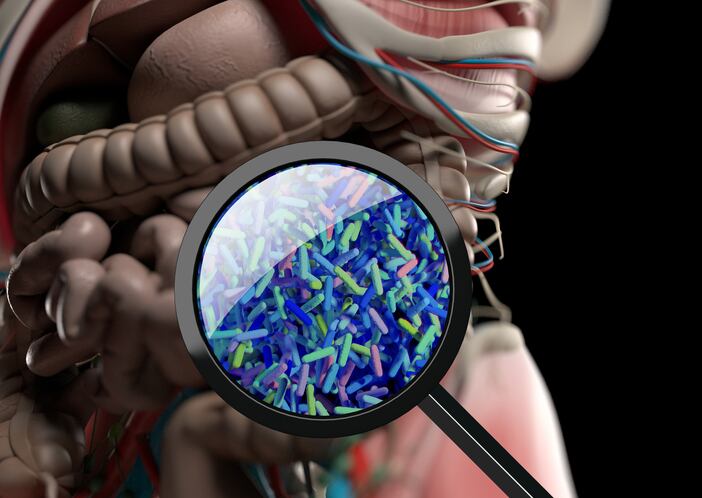
What changed in the gut
Microbiome analysis showed that the high-fibre group underwent larger shifts in overall community composition at week two versus the low-fibre control, based on weighted UniFrac distance, which gives more weight to abundant organisms.
By week four, the between-group difference on that metric had narrowed and was no longer statistically significant, but the trajectory still suggested ongoing modulation.
At the genus level, the high-fibre diet increased several short-chain fatty acid (SCFA)-associated groups.
Bifidobacterium rose significantly at weeks two and four in the high-fibre arm and was significantly higher than in the control at both time points. This is consistent with inulin’s well-known bifidogenic effect.
Anaerostipes and Fusicatenibacter also increased from baseline to week four in the high-fibre arm.
Functionally, Fusicatenibacter breaks down various sugars and produces lactate and acetate, which Anaerostipes can convert into butyrate, a key SCFA that nourishes colon cells and supports the gut barrier.
Faecal chemistry mirrored these shifts. The high-fibre group showed significant increases at week two in butyrate, iso-butyrate, and iso-valerate, aligning with the growth of butyrate-linked taxa.
These increases were not sustained at week four, suggesting a dynamic response influenced by day-to-day intake, adaptation, or individual variability.
Limited sleep and skin signals may improve with longer use
Sleep and skin outcomes remained secondary and exploratory. On average, neither sleep inventory scores nor most skin items changed meaningfully over four weeks.
However, the authors observed correlations between the abundances of Anaerostipes and Fusicatenibacter and some positive sleep and skin scores, along with small within-group improvements for a few skin items at interim timepoints.
These signals do not justify front-of-pack claims today but support a hypothesis that sustained, fibre-driven microbiome shifts could yield broader systemic benefits with longer exposure or higher doses.
Brands exploring gut-brain and gut-skin narratives should factor longer study horizons and more granular readouts into their evidence plans.
Limitations to weigh in evidence plans
Three design features should temper how these results extend to claims and product roadmaps. Firstly, the control foods included approximately 2g per day of fibre, which blurred the contrast and likely reduced between-group differences on some endpoints.
Secondly, the intervention lasted four weeks, which was enough for bowel habit changes and early microbial shifts but may have been too short to capture durable effects on sleep, skin, or metabolic markers.
Thirdly, the study used 16S rRNA sequencing, which profiles bacteria at the genus level and estimates relative abundance but does not resolve species, strains, or functional genes. Longer trials with metagenomics or metabolomics would help pinpoint pathways and strains responsible for benefits.
In conclusion, the researchers stated: “Although systemic outcomes like sleep and skin showed limited changes in the short timeframe, the microbial shifts we observed suggested that a longer intervention could potentially yield broader benefits via gut–brain and gut–skin pathways.”
Source: Microorganisms. 2025,13, 2068. doi: 10.3390/microorganisms13092068. “Effects of Dietary Fiber Supplementation on Gut Microbiota and Bowel Function in Healthy Adults: A Randomized Controlled Trial”. Ryo Inoue, et al.