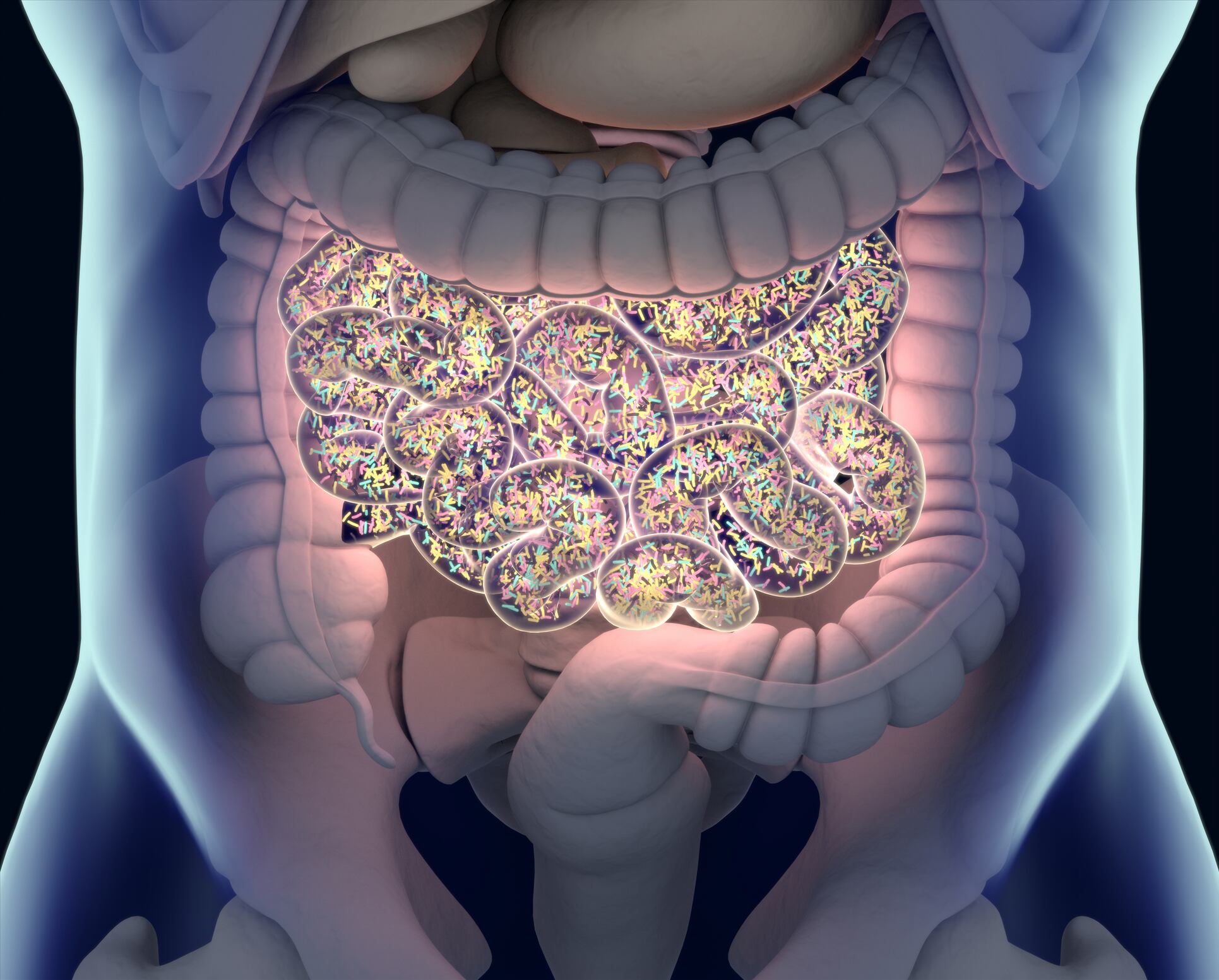
Recent studies have suggested there is an altered gut microbiota in IBS subjects compared with controls. However, the way in which the gut microbiota and IBS symptoms are linked mechanistically remains poorly understood. Diets avoiding fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAPs) have demonstrated efficacy (14-17) in reducing IBS symptoms.
The mechanisms are debated,18 but potentially involve modulation of microbiota composition and metabolite production.19 The low FODMAP diet is challenging for many patients to follow, often requiring increased time preparing meals, recipe adaptation and fewer options for convenience foods. Its long-term consequences on health are unknown. Thus, there is a recognised need to better understand how low FODMAP diets work,20 and ideally identify biomarkers that predict response.
The aim of the present study, conducted by researchers from The Wellcome Sanger Institute, UK, was to identify a biomarker of response to the low FODMAP diet and gain insights into microbial changes underlying treatment success using high resolution metagenomic and functional analysis of subjects with IBS and household controls before and while on a low FODMAP diet.
The study
A prospective single centre case–control study recruited participants recruited from outpatient clinics at Cambridge University Hospital in the UK. The study included adults (aged 18–68) meeting the Rome IV criteria for diarrhoea-predominant or mixed type IBS (IBS-D and IBS-M, respectively) with respective household controls.
Participants were assessed for suitability by a consultant and a dietitian. Three subsequent study visits were supervised by one of two senior gastroenterology dietitians trained and experienced in the administration of the low FODMAP diet. Seven-day food diaries (documenting the preceding week’s dietary intake) were collected from all participants and symptom severity scores captured using the IBS Severity Scoring System (IBS-SSS).27 Diet FODMAP scores were assessed using a previously published qualitative method (28).
Participants and their household controls were asked to provide a stool sample at visit 1 while on their usual diet, after 4 weeks on a low FODMAP diet (at visit 2) and 12 weeks following FODMAP re-challenge in subjects with IBS improving on the diet (to identify individual FODMAP triggers), or a return to usual diet in subjects with IBS not improving with the diet and in all household controls (visit 3). To profile the taxonomic composition of the stool samples from cases and controls, we performed shotgun metagenomic sequencing.
Results
A total of 41 IBS cases and their household controls followed a low FODMAP diet for 4 weeks and provided a stool sample while on the diet. There was no significant difference in FODMAP scores at baseline or on the diet between IBSP and IBSH clusters, and as expected, the scores fell significantly for each cluster on diet. There was a significant reduction in the IBS-SSS on the low FODMAP diet (mean IBS-SSS pre-diet=278, on diet=128).
This was observed both in patients harbouring IBSP and IBSH-type microbiomes but the difference in degree of response was more pronounced in IBSP patients.
IBS-SSS remained lower than at visit 1, 3 months after the completion of the low FODMAP diet. Thus, the shift in the IBSP microbiota to a heathy profile appeared stable for at least 3 months and correlated with continuing symptomatic well-being.
Comparison of taxonomic profiles between baseline (pre-diet) stool samples and those obtained while on the low FODMAP diet for 4 weeks revealed a significant shift in the microbiota composition of IBSP cases but not IBSH cases nor healthy controls.
The authors conclude that IBSP microbiomes were notably different from those of IBSH cases and healthy household controls, with an enrichment of distinct bacterial species and gene families seen in IBSP allowing them to propose potential pathogenic mechanisms.
Within the dysbiotic IBSP microbiomes, the team saw a significant enrichment of a broad range of Firmicutes species, including known human pathogens (C. difficile, C. sordellii and C. perfringens), a pathobiont associated with UC (Faecalicatena gnavus, previously named R. gnavus45) and known gut species not previously identified as human pathobionts (C. clostridioforme and Fusicatenibacter saccharivorans).
Interestingly, they also saw an enrichment in IBSP microbiomes of the lactic acid bacteria Streptococcus parasanguinis and Streptococcus timonensis that are usually found in the oral cavity.
At a functional level, IBSP microbiomes were enriched in genes and pathways involved in metabolising carbohydrates. This could lead to increased anaerobic glycolysis and associated carbon dioxide, hydrogen and methane production, and therefore increased IBS symptoms.
The authors note that limitations of this study include that limited sample size and the fact the dietary information was limited to the last week of the interventional phase of the low FODMAP diet.
They state: "Our findings of distinct IBS clusters based on microbiome profiles, the shift on the low FODMAP diet and the clinical responses, should be validated in other populations from different geographical distributions and exposed to different dietary habits.
"The identification of a microbial signature ‘biomarker’ that correlates with improved response to a low FODMAP diet may, if validated, allow better stratification and selection of patients likely to benefit from the diet. In IBSP subjects, there is the prospect to consider therapeutic strategies that manipulate the microbiota in the same direction and achieve the same symptomatic improvement but without the need to undergo the same stringent dietary restrictions.
"Further, closer study of the implicated microbes may give the opportunity to better understand the interaction between diet, microbiota, metabolites and the human gut-brain axis that leads to the development of IBS symptoms in more than 10% of the world’s population."
Source: BMJ Gut
Vervier K, et al
"Two microbiota subtypes identified in irritable bowel syndrome with distinct responses to the low FODMAP diet"
doi:10.1136/gutjnl-2021-325177